Safe Sex: The Millennial Problem
September 27, 2017
With so much information at our fingertips, why is safe sex still an issue in practice?
Romance was just a swipe away for Louis, a 22-year-old student at Fresno City College. Fresh out of a long-term, serious relationship, Louis knew that he wasn’t looking for love, but rather, someone to pass the time with.
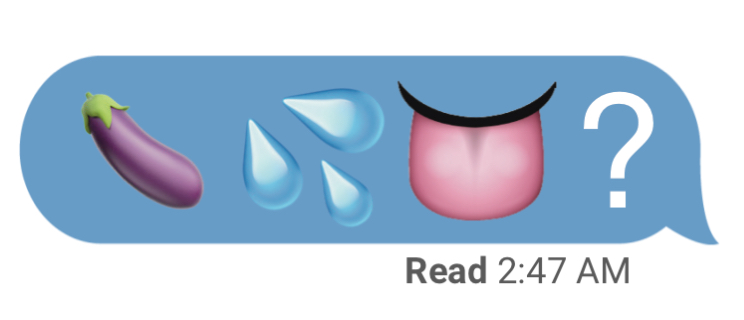
He took to the dating app Tinder and eventually met Ava, a 21-year-old student, whom he hit it off with fairly quickly. The two exchanged numbers and began texting, eventually sending each other risque photos and sexting. The next day, they met at his apartment, and after a few drinks to loosen up, they had sex.
In the heat of the moment, Louis and Ava were reluctant to stop to get a condom, and instead engaged in unprotected sex. Louis’ case is like many others’ his age: a shocking amount of millennials don’t use condoms all of the time.
According to the 2017 SKYN Condoms Millennial Sex Survey, 60 percent of millennials who are currently in college (age 18-24) are having sex at least once a week, but only 54 percent of them are using condoms “always” or “most of the time.”
College provides a great opportunity for young adults to experiment with sex. For those who choose to experiment, practicing safe sex is common knowledge. So why is it that only a little over half of college students use condoms consistently and effectively?
“Of course sex feels better without them [condoms], but it’s still important to use them nevertheless,” said Josh, a 22-year-old FCC student. “Although if I do end up in a serious relationship with someone I trust, I’ll eventually stop using condoms with them.”
Josh says that being in college has provided both a negative and positive outcome for his sex life. Although college has provided the opportunity to meet different people, many students are too busy to form a “real relationship” and opt for simply hooking up instead.
“It’s OK to sleep around and experiment with your sex life at this age,” said Shelby, a 20-year-old student at FCC. “I always use a condom if I’m sleeping with someone for the first time, even though I’m on birth control.”
Shelby claims that her high school did not offer an adequate sex education program, and the optional course was eventually phased out of the curriculum entirely. The same goes for Drew, a 21-year-old FCC student.
“I never really learned about all of the different kinds of birth control, other than condoms and the pill, until years after my high school sex ed class,” said Drew. “There’s a lot more that I’ve learned in experimenting and just going through life.”
According to a recent Public Religion Research Institute research study, 23 percent of millennials report they did not have a sex education class in middle or high school.
Additionally, 37 percent of millennials say that sex education classes were not helpful to them in making decisions about sex and relationships.
“Condoms are definitely important, even if a woman is on another form of birth control,” said Drew. “Condoms should still be used to prevent from STIs. It’s a little more reassuring to have two forms of birth control working at the same time.”
Sexually transmitted infections, or STIs, are defined as any infection that is characteristically transmitted by sexual contact and may either clear up or develop into a sexually transmitted disease.
The American Sexual Health Association (ASHA) states that one in two sexually active persons will contract an STI by age 25. Even though young people account for half of new STI cases, a recent survey showed only about 12 percent were tested for STIs in the last year.
The ASHA statistics also show that rates of the three most common STIs—chlamydia, gonorrhea and syphilis—reached a record high level, with approximately 1.5 million cases in 2015. Those aged 15 to 24 years old accounted for 65 percent of chlamydia diagnoses and 50 percent of gonorrhea diagnoses.
“Not a lot of people will ask the person they’re hooking up with when the last time they got checked for STIs was, so it’s important to use condoms just in case,” said Shelby. “It’s not just about not getting pregnant.”
According to the California Department of Public Health, the number of reportable STIs in the state is at a 20-year high, with nearly 250,000 cases as of 2015. Fresno County has some of the highest STI rates in the state, with over 10,000 affected by chlamydia, gonorrhea, and early latent syphilis.
Lisa Chaney, the Health Services Coordinator at FCC, encourages students to come to the health services for any questions they might have regarding their sexual health.
“We provide counseling about birth control methods available, and encourage students to go to a [medical] provider so they can decide what’s best for them,” said Chaney. “Students can come here and really ask all of the questions they wonder about and get good answers to help them make good decisions about their own sexual health.”
Student Health Services at FCC is located in the student services building, room 112. Although they don’t offer STI testing on campus, Health Services brings in HIV and HEP-C testing to their office on the second Wednesday of each month.
“Some people are reluctant to seek information, said Chaney. “We try to destigmatize the negative stigma surrounding STIs and encourage people to seek medical treatment if there’s a concern.”
Although getting tested for STIs may seem intimidating, the process for most tests is fairly simple, consisting of either a blood or urine sample. Many STIs are curable or have some sort of medical treatment available to ease the symptoms.
Of course, it is always easier to prevent an STI than it is to treat it; latex condoms are highly effective against the transmissions of most STIs when used correctly, according to the Center for Disease Control and Prevention.
“Sometimes we get distracted by how fast-paced things are going and just forget to use protection,” said Louis. “Hooking up is fun, but we really should be more careful.”